Sunday, September 26, 2021
International Daughter's Day: Stubborn Mother 2.
Tuesday, September 21, 2021
Over Hydration!!!
©2017 Am Ang Zhang
Ancient Remedy: Modern Outlook
Chinese farm workers have always worked in the heat of the fields but heat stroke seems to be rather uncommon. I wonder if our dried preserved plum has something to do with this.
It has to be said that the diet of many such Chinese workers was generally higher in sodium, from dried salted fish and vegetables. It is likely that the serum sodium of many such workers would have been at the high end of the normal range. Modern advice on cutting down sodium often does not take account of sweating in hot countries. A friend of mine with hypertension had an epileptic seizure when he went to work in Singapore. Luckily the medical services there were alert to the problem and he survived. He was on a low sodium diet and on diuretics amongst other medications.
I also remember one very hot August day when we hiked down Grand Canyon to Angel Point. There were warnings everywhere of the risks and even fatalities on such walks. The National Park did have clean drinking water taps along the way and one particular girl overdid the drinking. She had a narrow escape, as the Ranger fortunately knew a thing or two about rehydration. He put some salt in a can of Sprite and reverted a potentially serious situation.
When the first public golf course was opened on the beautiful island of Kau Sai Chau in Hong Kong, drinking water was provided along the course. One player drank so much that he nearly died of water intoxication (result of drinking excessive amounts of plain water which causes a low concentration of sodium in the blood leading to amongst other problems: ‘brain’ swelling---cerebral oedema). Marathon runners are at greater risk than most as reported by the New England Medical Journal. There have been other notable cases of water intoxication elsewhere. I remember one of my professors telling us: the body survives dehydration much better than drowning. How right he was, as water intoxication is in a sense a kind of drowning.
The first time we went to Thailand the most amazing dip was simply a bowl of sugar that has been mixed with salt and some chopped chilies for good measure. This dip was used for serving unripe mangoes, papayas, guavas and other local fruits, and gave me a taste sensation that was unforgettable. Same principle as ORT.
In Thailand, workers in rice fields, fruit orchards and vegetable patches manage to survive temperatures of over 100°F.
On the other hand, Chinese dried plums are such neat, little, easy to carry things. Perhaps we should try to popularize this ancient remedy for the benefit of all. Be warned, only those made with sugar and salt work, not the ones with artificial sweeteners.
I well remember
Of 766 runners enrolled, 488 runners (64 percent) provided a usable blood sample at the finish line. Thirteen percent had hyponatremia (a serum sodium concentration of 135 mmol per liter or less); 0.6 percent had critical hyponatremia (120 mmol per liter or less). On univariate analyses, hyponatremia was associated with substantial weight gain, consumption of more than 3 liters of fluids during the race, consumption of fluids every mile, a racing time of >4:00 hours, female sex, and low body-mass index. On multivariate analysis, hyponatremia was associated with weight gain (odds ratio, 4.2; 95 percent confidence interval, 2.2 to 8.2)....
Latest:
Loquat, Winter Melon & Sapote
This Child Psychiatrist also uses the Stethoscope
This was from 2008!
Sunday, September 19, 2021
N95 Masks: Medical Heresy from Plague to SARS-CoV-2
- March 10, 2021
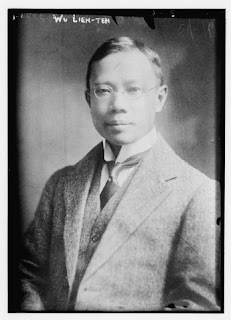
Dr. Wu Lien-teh's 142nd Birthday
Google Doodle celebrates the 142nd birthday of Chinese-Malaysian epidemiologist Dr. Wu Lien-teh, who invented a surgical face covering that is widely considered the precursor to the N95 mask.
Google honoured Dr Wu Lien-teh, a Chinese Malaysian epidemiologist who discovered the N95 mask over a hundred years ago, with a personal artwork on their search graffiti.
Portrait of Dr. Wu Lien-teh, circa 1910-1915. (Courtesy of the Library of Congress PPOC.)
Link: https://www.google.com/doodles/dr-wu-lien-tehs-142nd-birthday
The ultimate price of foolish arrogance
One very arrogant French doctor by the name of Mesny arrived a week later than Dr Wu at Harbin. Dr Wu paid him a courtesy call and briefed him of the results of his own initial investigation of the disease and the importance of wearing special protective face mask. This is the extract from Dr Wu’s own writing,
The Frenchman was excited, and kept on walking to and fro in the heated room. Suddenly, unable to contain himself any longer, he faced Dr Wu, raised both his arms in a threatening manner, and with bulging eyes cried out “You, you Chinaman, how dare you laugh at me and contradict your superior?”
Dr Wu replied, “I am sorry, Dr Mesny, that our talk intended by me to be a friendly one, should lead to such unpleasantness.”] (Page 19 of Dr Wu's Autobiography)
Dr Wu then left the place.
Dr Mesny later visited another hospital operated by the Russians. He examined a few infected patients without wearing a mask against the advice of Dr Wu. A few days later, he was infected with the pneumonic plague and died 6 days after he examined the infected patients without wearing a protective mask. The ultimate price of blind and foolish arrogance.
Dr Wu’s Philosophy
“I have emphasized the need of faith, perseverance and originality: the first, because without it during troublous times we would simply have to throw up one’s hands and despair: the second, because no great scientific or medical benefit has yet been achieved without thorough attention to accuracy and details; the third, because with a conservative education handed down for 4000 years like ours, it is most essential for our minds to branch out in new directions so as to cope successfully with the progressive tendencies of the times.”
“But in order to achieve the quickest and most permanent results in the most economical way, her leaders should absorb the best that the West can offer, such as, seriousness of purpose, service to others as well as self, a scientific temperament, rigid scrupulousness in management of business undertakings, attention to detail and a willingness to learn from outsiders even at the height of success. On the other hand, they should eschew the weaker points of western civilization, such as, undue worship of material success at the expense of the soul, over-indulgence in the ordinary comforts of life and luxuries, and lack of discipline in the family.”
Link: https://discover.hubpages.com/education/The-Pioneer-Plague-Fighter-Dr-Wu-Lien-Teh
Underclass: The Old Beggar
Tuesday, September 14, 2021
NHS & Gawande: Morbidity and Mortality Conference M+M
The GMC warned that the safety of hospital patients is being put at risk because inexperienced young doctors are too often being left in charge of A&E and other units. We need to look at the way medical liability is covered in Hospitals where indeed all juniors must be covered by a consultant in one way or another. The responsibility would indeed be that of the hospital management and not on the poor Junior Doctor. The difficulty is the choice between NO doctor or a less experienced one. Should the patient be told or should the A&E just be closed? Will management do that or just continue to abuse the poor juniors and blame them when things go wrong. No wonder my friends' children prefer to become lawyers.
>>>See also Dr No: We Have No Black Boxes
Quotes
- ‘There have now been many studies of elite performers – international violinists, chess grand masters, professional ice-skaters, mathematicians, and so forth – and the biggest difference… is the cumulative amount of deliberate practice they’ve had.’
- ‘We have long faced a conflict between the imperative to give patients the best possible care and the need to provide novices with experience. Residencies attempt to mitigate potential harm through supervision and graduated responsibility. And there is reason to think patients actually benefit from teaching. Studies generally find teaching hospitals have better outcomes than non-teaching hospitals. Residents may be amateurs, but having them around checking on patients, asking questions, and keeping faculty on their toes seem to help. But there is still getting around those first few unsteady times a young physician tries to put in a central line, remove a breast cancer, or sew together two segments of a colon… the ward services and clinics where residents have the most responsibility are populated by the poor, the uninsured, the drunk, and the demented… By traditional ethics and public insistence (not to mention court rulings), a patient’s right to the best care possible must trump the objective of training novices. We want perfection without practice. Yet everyone is harmed if no one is trained for the future. So learning is hidden behind drapes and anesthesia and the elisions of language.’
- ‘There is one place, however, where doctors can talk candidly about their mistakes, if not with patients, then at least with one another. It is called the Morbidity and Mortality Conference – or, more simply, M+M – and it takes place, usually once a week, at nearly every academic hospital in the country. This institution survives because laws protecting its proceedings from legal discovery have stayed on the books in most states, despite frequent challenges.’
















6 comments:
Anna :o]
... but I never liked the word 'underclass' ... or 'subhuman', two of the same vocabulary, because of the degradation to humanity that is associated with such expressions. Surely, humanity with all it's ills, is still less vicious than that, or am I underestimating our 'exclusive' arrogance?
Well done, as usual, CC, you've made me think, and stirred some emotions :-)
I am glad you liked the portrait. Photography portraiture is difficult as it was only a split second thing unlike painting which often takes many sittings (painting from photo is the modern way and that is why much of the BP stuff is not good in my humble opinion.
Saw One Man, Two Guvnors at the National: all the classes were bad----Public School class, butler class, mafia class, lawyer class, waiters class.
... one of the most amazing, and very disturbed, paintings done from a photo, is [Gorky's mother and child]. He was influenced by Cezanne and Picasso, but that painting has something, a life of it's own, despite it's artist death long ago ... I find it scary and very disturbing ... Gorky needed you CC, check him out :-)
It is the same with many Catholic countries and Portugal is one of them.
He was given some bread so from under his seat he pulled out some raw garlic cloves and ate the bread with it. He is going to live a long life.
My old man was doing good, much good.
COI: I did give him some money, after the photo of course.